News
Pain Clinic case study
18th November 2021

Joanne Michou VETMB MA DIPECVAA MRCVS, RCVS and European Specialist in Veterinary Anaesthesia and Analgesia
Here we present a pain clinic case report that demonstrates how our teamwork in anaesthesia and pain management, neurology, orthopaedics and physiotherapy come together to give a successful outcome for the patient and owner.
Pain clinic cases can be extremely rewarding but also challenging. They are often older patients, with multiple co-morbidities, multiple sources of pain, who are frequently intolerant of certain drug therapies. They may have been ‘trialling’ drug therapies that seem not to work and the history is often such that it takes much longer than is often given in the tight consult times of general practice. There are also often very strong emotive ties for the owner to certain behaviours and activities.
Meet Harry. Harry was an eight-year-old, 33kg male neutered Labrador-cross breed who initially presented to our neurology and orthopaedic services as the owner noted that Harry was acutely reluctant to sit down and seemed in pain. He also had a history of chronic elbow disease, thickened stifles and was prone to gastro-intestinal upset with NSAID’s.
Harry’s owners were very dedicated and keen to perform diagnostics and discuss treatment options thereafter to give Harry the best quality of life. After initial assessment, one of our anaesthetists prepared him for general anaesthesia and our radiography team performed radiographs of the pelvis and stifles, CT of the thoracic limbs and MRI of the lumbosacral spine.
 Harry was found to have chronic severe bilateral elbow osteoarthritis, bilateral degenerative carpal and metacarpo-phalangeal joint osteoarthritis, very minor right stifle degenerative joint disease and a non-compressive lumbosacral disc protrusion. With the severity of the elbow disease and multiple joints affected, medical management was deemed most appropriate. Harry was discharged to return two weeks later for assessment in the pain clinic to assist with ongoing management. He had been prescribed memantine, gabapentin and paracetamol and alteration and restriction in exercise regime.
Harry was found to have chronic severe bilateral elbow osteoarthritis, bilateral degenerative carpal and metacarpo-phalangeal joint osteoarthritis, very minor right stifle degenerative joint disease and a non-compressive lumbosacral disc protrusion. With the severity of the elbow disease and multiple joints affected, medical management was deemed most appropriate. Harry was discharged to return two weeks later for assessment in the pain clinic to assist with ongoing management. He had been prescribed memantine, gabapentin and paracetamol and alteration and restriction in exercise regime.
After an introduction and briefly explaining my role within the hospital as an anaesthetist and specialist in pain management, I started by collecting a detailed history.
Prior to being seen at Lumbry Park, Harry had a variety of therapeutic interventions over the years including elbow arthroscopy, two steroid LS epidural injections, platelet-rich plasma in carpi and elbow joints, physiotherapy and hydrotherapy, a course of cartrophen injections, and a variety of analgesic agents including paracetamol, tramadol, NSAID’s including meloxicam, carprofen, robenacoxib and previcox. He had a history of GI upset, particularly with NSAID’s.
The main presenting complaint was that Harry did not want to sit down and seemed uncomfortable. The owners were worried about his quality of life and that he seemed in pain.
The owners thought there had been no improvement since he was seen three weeks ago, although they had not started the medications dispensed as they were concerned regarding the possible side effects. The owners found it hard to follow the exercise plan and keep him on lead as he was so full of energy and once he was off lead he ran into the bushes, swam in the sea and chased squirrels.
The owners had lots of questions about the medication he had been given and also other questions from research they had found, including a relatively new drug, bedinvetmab, and why the data sheet for the memantine was targeted at use in humans for cognitive dysfunction.
I discussed with the owners at length the basic pain pathway, how different drugs act and the importance of needing to start analgesia in patients with chronic pain. We discussed how acupuncture works and how patients may be responders or non-responders, QOL versus side effects of drugs and using multimodal analgesia to minimise side effects, the side effects of different drugs and importance or lack of importance of some. For example, some dogs will vomit with amantadine, but this this caused by a sudden surge in dopamine levels and this is not particularly worrying and very different to vomiting that may occur with an intolerance to NSAID’s because of effect on prostaglandins and GI mucosa. Vomiting with amantadine is easily remedied by giving it with food which slows absorption and reduces the peak of dopamine. We discussed licensing and that many drugs, including the memantine, are not licensed for use in dogs. Importantly, we discussed owner’s expectations, that long term management is required and it will likely be a combination of drug therapy and physical therapies with monitoring for improvement, plateau or deterioration.
Examination revealed a marked forelimb lameness, worse on the left than the right, myofascial triggers points particularly over the right lumbar paraspinals and responsive to even gentle sensation over the elbows. I recommended trying a non-invasive pain management plan, including acupuncture initially once a week. I recommended modulation of exercise with very specific instructions to avoid any room for interpretation. This is a balance between the owner and pet’s emotional wellbeing and avoiding exacerbation of the disease.
The owners still had concerns regarding grapiprant, so after ensuring there were no side effects from the memantine and gabapentin, we started the grapiprant a week later as Harry was still in some discomfort.
By the third week the owners had noticed significant improvement. Harry continued to improve thereafter, although there were times of acute deterioration. With some investigation, it was often found to be linked to a specific type of activity or length of exercise.
Six months after his first pain clinic consultation, Harry is doing brilliantly. His owners are thrilled and believe this is the best he has been in a very long time. He is now undergoing acupuncture once every five weeks, seen our wonderful physiotherapist who has helped the owner learn how to perform massage and he is now only receiving grapiprant.
In my experience, building a rapport with the owners who have often had many appointments sometimes at multiple veterinary practices for the same conditions, is of vital importance for them to trust. Quite often there is a need from the owners to understand which also helps aid exercise, activity and drug compliance.
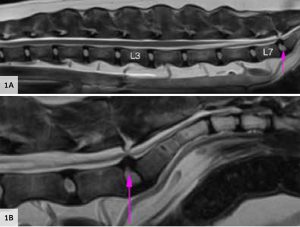
Figure 1A and 1B: MRI sagittal T2WI of the lumbosacral spine showing mild protrusion of the intervertebral disc at the lumbosacral area producing partial loss of the epidural fat, with no evidence of caudal equina displacement or compression (pink arrow). Symmetrical and normal appearance of nerve roots.
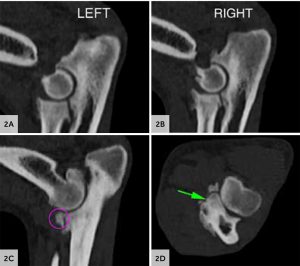
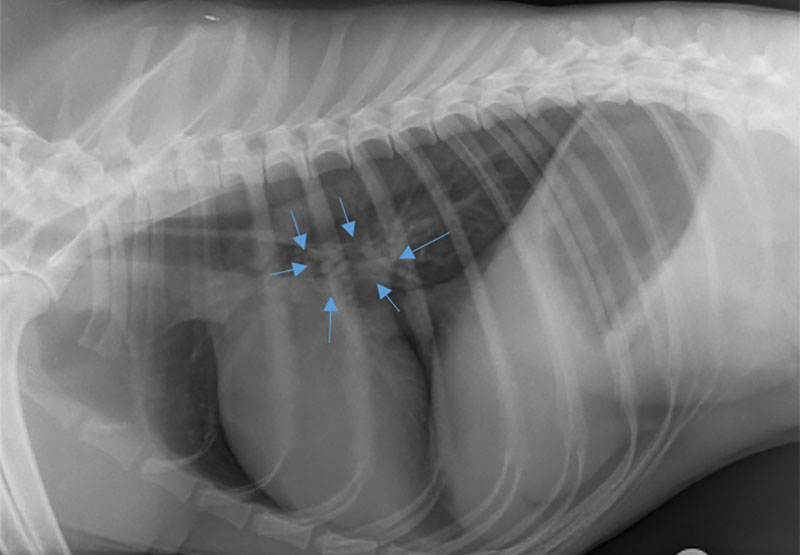
Figures 2A, B, C and D: CT of the elbows shows bilateral joint effusions, moderate periarticular new bone formation affecting both elbows. The right medial coronoid process has an irregular surface with new bone formations. The left one has a flattened surface and moderate sclerosis of the adjacent bone that extends towards the radioulnar incisure (green arrow). Presence of several mildly displaced articular fragments (pink circles).
Back to news & events