Coco, a 5-year-old Dachshund, faced a sudden challenge – progressive weakness in her back legs and back pain. Having previously recovered well from a similar issue in 2022 at Lumbry Park Referrals, she returned for expert care.

Expert Diagnosis:
Our neurology team performed a thorough examination and identified the issue: a problem in her thoraco-lumbar spine.
Read on for the detailed Case History; Physical and Neurological examination; Differential Diagnoses; Diagnostic Imaging Findings; Treatment and Outcome:
History:
Coco, a 5-year-old female neutered, Dachshund cross dog, 8kg, was presented as an emergency with a 6-day history of acute and progressive pelvic limb proprioceptive ataxia and paraparesis. Inappetence and spinal pain were also reported. Coco was being treated with gabapentin and meloxicam. There was a previous clinical history of a L2-3 intervertebral disc extrusion treated surgically in 2022 at Lumbry Park from which Coco recovered fully.
Physical and Neurological examination:
Coco was borderline ambulatory as she was not able to perform 10 steps without collapsing. There was pelvic limb proprioceptive ataxia and moderate paraparesis paresis. The muscle tone of the pelvic limbs was normal. Postural responses including paw placement and hopping were absent bilaterally. Segmental spinal reflexes – flexor-withdrawal and patellar reflexes – were unremarkable. The cutaneous trunci reflex was interrupted around L1. There were behavioural signs of discomfort in the thoracolumbar region. The remaining neurological examination was unremarkable.
Physical examination was unremarkable.
Neurolocalisation:
T3-L3 spinal cord segments.
When assessing a dog or a cat with gait abnormalities of a suspected neurological origin it is essential to differentiate between upper motor neuron (UMN) and lower motor neuron (LMN) lesions. Typically, UMN lesions result in loss/reduction of motor function, spinal reflexes that are normal to increased in the spinal cord segments caudal to the lesion and increased muscle tone caused by a disinhibition effect that the UMN has on LMNs caudal to the lesion. In contrast, LMN lesions result in flaccid paresis with weakness in weight-bearing or a short-stride gait, spinal reflexes that are decreased in the spinal cord segments affected and reduced muscle tone.
When considering a spinal cord disease, the segments are divided in C1-5, C6-T2, T3-L3 and L4-S3. In our case, given only the pelvic limbs were affected we considered T3-L3 versus L4-S3. The presence of normal muscle tone, normal spinal reflexes, normal anal sphincter and tail tone led us to localise T3-L3 SCS. This was collaborated by the cutaneous trunci cut off.
Differential Diagnoses:
Using the VITAMIN D mnemonic and the signalment, onset and progression of the dog we considered the following differentials as most likely:
Vascular: x.
Inflammatory/ Infectious: Discospondylitis, empyema, meningomyelitis of unknown origin, infectious meningomyelitis.
Traumatic, Toxic: traumatic disc herniation, Toxin such as anti-epileptic drugs (i.e. KBr).
Anomalous: spinal intra-arachnoid diverticula, constrictive myelopathy.
Metabolic: x
Idiopathic: x
Neoplastic: primary and secondary.
Degenerative: Intervertebral disc herniation.
Diagnostic tests:
Haematology and biochemistry were within reference intervals.
A CT scan of the vertebral column revealed a well-defined, extradural, hyperattenuating material within the right side of the canal causing marked compression of the spinal canal and deviation of the spinal cord towards the left at the level of the L1 vertebral body. This material was continuous with the intervertebral disc space at T13-L1. These changes are compatible with a T13/L1 disc extrusion.
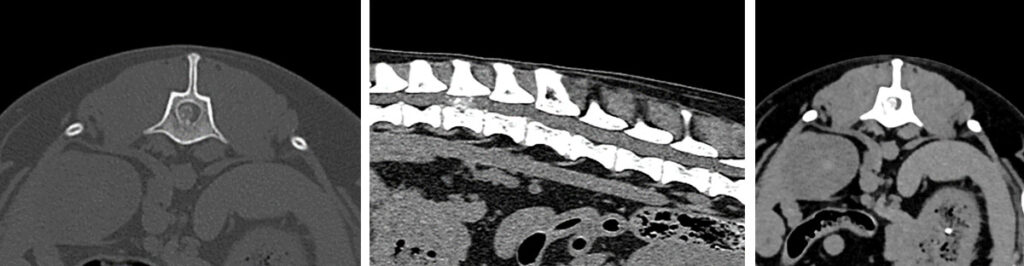
MRI scan, CT scan and CT scan myelogram are used for diagnosis of intervertebral disc extrusion. In chondrodystrophic dogs with mineralized discs a CT scan can be seen as a first-line imaging modality for dogs presenting with thoracolumbar myelopathy. In Dachshunds, a non-contrast CT is a sufficient imaging modality for intervertebral disc disease and surgical planning in the majority of cases (96.4%; 323/335) (Emery et al., 2018).
Diagnosis: T13-L1 intervertebral disc extrusion
Treatment and outcome:
An ultrasound-guided erector spinae plane block was performed with bupivacaine to provide local analgesia and to reduce the need of intraoperative pharmacological interventions and to reduce opioid consumption post-operatively.
A right sided dorsolateral approach to the T13-L2 disc spaces allowed a T13-L1 mini-hemilaminectomy to be carried out, this window was extended to the L1-2 foramen to remove any extruded material from around the nerve root. Fenestration of the T12-13 and T13-L1 disc sites was carried out.
Coco was hospitalised for two days for multimodal analgesia, pain scoring, strict exercise restriction and for neurological assessment. Upon discharge, Coco was ambulatory with mild pelvic limb ataxia, normal paw placement on the right pelvic limb and mildly reduced on the left pelvic limb. Segmental spinal reflexes were intact and Coco was urinating independently.
Surgical outcome for non-ambulatory dogs with intervertebral disc extrusion is usually good (93%, 341 dogs). Fenestration of the herniated disc space at the time of surgical decompression minimises the risk of re-extrusion and possibly the risk of reoccurrence in multiple site fenestration. Importantly, the risk of recurrence is higher for dachshunds (25%) which is a consideration in the surgical management of these dogs.
Acknowledgments:
Thank you to Dr. Rebecca Taylor and team at Anton Vets for referring Coco.
All the staff at Lumbry Park Veterinary Specialists.
We have a fantastic team of people who work at Lumbry and this combined with our brilliant facilities means we can see any of your neurological emergencies. Our neurology team is composed of eight neurology clinicians as part of our Specialist-led team. Our multidisciplinary approach means patients at Lumbry can have specialist led anaesthesia input (including local analgesia techniques (e.g. ultrasound-guided erector spinae plane block)) and our neurology team is vastly experienced and able to perform diagnostics and offer surgical interventions for any neurological condition. Last, but not least, our nurses and support staff ensure our care is maintained at the highest possible standards throughout the patient journey to ensure you and your patients receive an excellent referral experience.
References:
Viilmann, I., Drozdzynska, M. & Vettorato, E. Analgesic efficacy of a bilateral erector spinae plane block versus a fentanyl constant rate infusion in dogs undergoing hemilaminectomy: a retrospective cohort study. BMC Vet Res 18, 423 (2022). https://doi.org/10.1186/s12917-022-03523-x
Emery, L., Hecht, S. & Sun, X. Investigation of parameters predicting the need for diagnostic imaging beyond computed tomography in the evaluation of dogs with thoracolumbar myelopathy: Retrospective evaluation of 555 dogs. Veterinary Radiology & Ultrasound. 59(2), 147–154 (2018). DOI: https://doi.org/10.1111/vru.12576
Olby NJ, Moore SA, Brisson B, et al. ACVIM consensus statement on diagnosis and management of acute canine thoracolumbar intervertebral disc extrusion. J Vet Intern Med. 2022; 36(5): 1570-1596. doi:10.1111/jvim.16480


