Summary:
An 8-year-old Poodle presented to our hospital with lethargy, anorexia, and jaundice. Despite initial investigations, the patient unfortunately had a cardiac arrest before a definitive diagnosis could be established.
Prior to the patient’s passing, our team conducted a thorough examination, including echocardiography. The results revealed significant cardiac abnormalities, including dilation of the right heart chambers and evidence of pulmonary hypertension (high blood pressure in the pulmonary artery).
While the underlying cause of the pulmonary hypertension could not be definitively determined, this case underscores the importance of prompt veterinary care and the complexity of diagnosing heart conditions in pets. Early intervention can improve outcomes and potentially prevent further complications.
Case details:
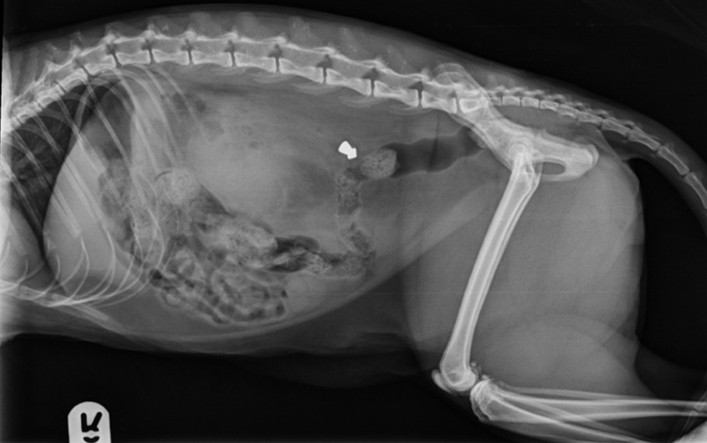
An 8-year-old female neutered Poodle presented collapsed and non-ambulatory after 3 days of anorexia and lethargy, with a tentative diagnosis of pancreatitis from the referring practice and poor response to intravenous fluid therapy, opioid analgesia and paracetamol. She was mildly pyrexic, jaundiced and had a heart rate of 96 bpm, with no cardiac murmur, and mild tachypnoea at 40 breaths per minute. The heart rate was considered anomalous with the rest of the clinical examination, thus an ECG was performed, demonstrating an idioventricular rhythm.
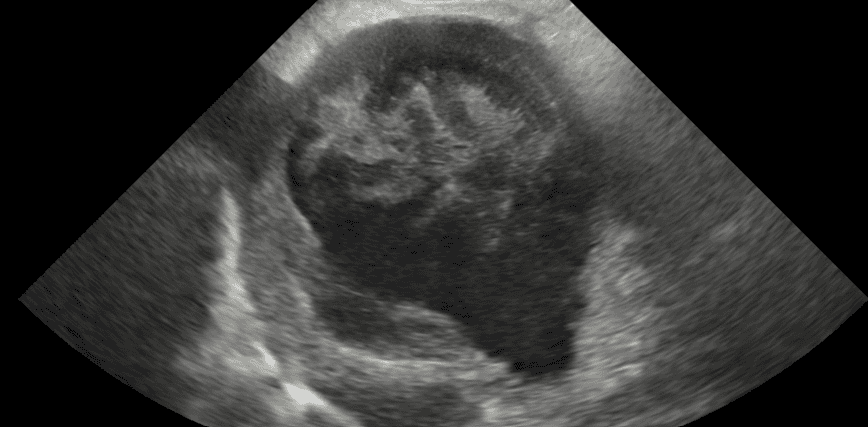
Echocardiography demonstrated dilation of the caudal vena cava (CVC), right atrium (RA) and right ventricle (RV) with thrombi and spontaneous echo contrast. The RV internal diameter in diastole was similar to the diameter of the LV, with significant paradoxical septal motion visible on both 2D and M-mode views. There was no regurgitant flow across the pulmonary or tricuspid valves. The pulmonary acceleration time/ ejection time was reduced to 0.3 (normal 0.5). A high probability of pulmonary hypertension was indicated as per the ACVIM Consensus Statement Guidelines for Pulmonary Hypertension in dogs 2020.
Further investigations were planned: haematology, biochemistry, C-reactive protein, D-dimer, clotting times, pancreatic lipase, thoracic and abdominal CT. Unfortunately the patient had a cardiac arrest during the thoracic CT, so identification of the underlying pathology was not determined. Due to the acute nature of the pulmonary hypertension and the presence of thrombi within the right atrium, the working diagnosis was type 4a pulmonary hypertension secondary to thromboembolic disease.
Pulmonary thromboembolism (PTE) is not a common diagnosis, with a wide range of underlying pathologies. If PTE is suspected or confirmed, treatment with antithrombotic medication should be started with heparin and rivaroxaban (a direct anticoagulant is preferred to antiplatelet agents such as clopidogrel and aspirin).
Quote/Clinician’s take-away or advice: As this case demonstrates, pulmonary thromboembolism can be a devastating condition. Prompt diagnosis and treatment with anticoagulation therapy are essential for improving patient outcomes. Veterinarians should be aware of the clinical signs and risk factors for this disease.
Supporting Visuals:
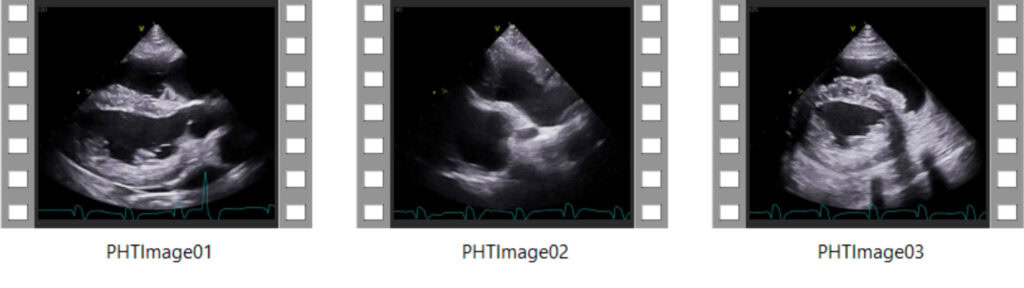
01: Right parasternal 5 chamber long axis view demonstrating the dilated right atrium and right ventricle.
02: Right parasternal long axis view focused on the dilated right atrium and caudal vena cava, with thrombomboli.
03: Right parasternal short axis view at the level of the ventricles demonstrating the flattening of the interventricular septum.